Fatal Disseminated Herpes Simplex in a very premature neonate
Keywords:
Pathology, Infant, Newborn, Premature birth, Herpes Simplex, Pregnancy Complications, Infectious, Neonatal Sepsis, Intranuclear Inclusion Bodies, InfantLow Birth WeightAbstract
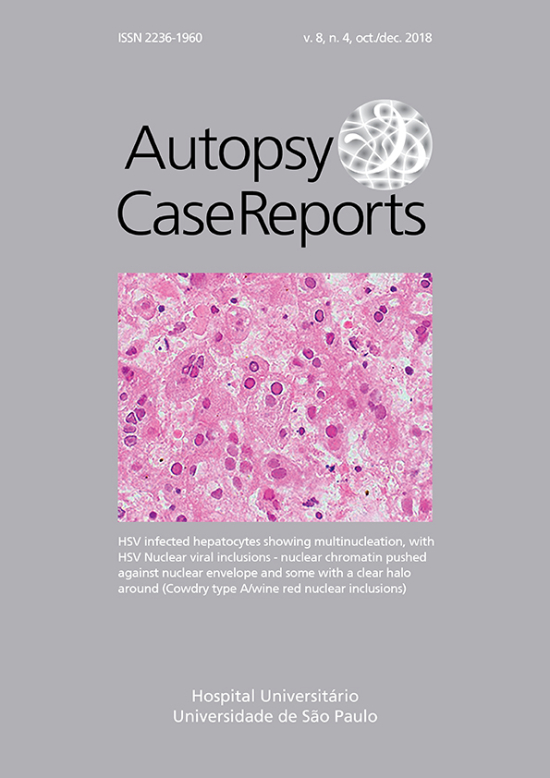
Herpes Simplex Virus infections (HSV) are ubiquitous. The neonatal HSV infection (NHSV) is rare. The incidence is estimated globally at only 10.3 per 100,000 births, but it can cause devastating disease in premature infants. Both HSV-1 and HSV-2 can be the etiologic agents in this type of vertically transmittted NHSV infection. Here we describe the pathological findings from a complete autopsy of a very low birth weight infant who succumbed to the infection despite early institution of antiviral treatment. We urge more awareness of this disease with continued surveillance; every effort should be taken to make an early diagnosis and thus prevent this devastating disease.
Downloads
Published
Issue
Section
License
Copyright
Authors of articles published by Autopsy and Case Report retain the copyright of their work without restrictions, licensing it under the Creative Commons Attribution License - CC-BY, which allows articles to be re-used and re-distributed without restriction, as long as the original work is correctly cited.