Co-infection of disseminated histoplasmosis and tuberculosis in an AIDS patient
DOI:
https://doi.org/10.4322/acr.%25y.75887Keywords:
Histoplasmosis, Tuberculosis, Acquired Immunodeficiency Syndrome, Autopsy.Abstract
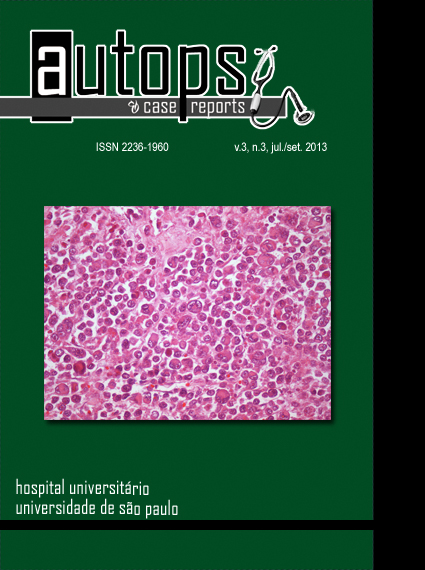
Histoplasmosis is a fungal disease caused by the dimorphic fungus Histoplasma capsulatum, recognized as an AIDS-defining illness since the Center for Disease Control’s revision criteria in 1985. This infection is reported to be present in 5-20% of AIDS patients, and in 95% of the cases it is manifested in its disseminated form. Serum antibodies and/or antigen research can make diagnosis, but the demonstration of the agent by culture or histopathological examination remains the gold standard methods. Co-infections in patients with AIDS are well known; however, reports on disseminated tuberculosis and histoplasmosis are scarce. The authors report the case of a female patient who presented a short-course history of weight loss, fever, and mild respiratory symptoms, with hepatosplenomegaly and lymphadenopathy. Laboratory workup called attention to anemia, altered liver, canalicular enzymes, liver function tests, high titer of lactate dehydrogenase (LDH), and pulmonary nodules on thoracic computed tomography. Incidental finding of yeast forms within the leukocytes during a routine blood cell count highlighted the diagnosis of histoplasmosis. The patient started receiving amphotericin B but succumbed soon after. The authors emphasize the possibility of this co-infection, the diagnosis of severe infection through the finding of yeast forms within peripheral leukocytes, and for the high titer of LDH in aiding the differential diagnosis.Downloads
Download data is not yet available.
Downloads
Published
2013-10-02
Issue
Section
Article / Clinical Case Report
License
Copyright
Authors of articles published by Autopsy and Case Report retain the copyright of their work without restrictions, licensing it under the Creative Commons Attribution License - CC-BY, which allows articles to be re-used and re-distributed without restriction, as long as the original work is correctly cited.
How to Cite
Tomazini, B., Bandeira, R., Aragão, T., Borges, J. C. A., Sasdelli, R., Salgado, V. P., Campos, F. P. F. de, & Lima, P. P. de. (2013). Co-infection of disseminated histoplasmosis and tuberculosis in an AIDS patient. Autopsy and Case Reports, 3(3), 49-58. https://doi.org/10.4322/acr.%y.75887