Hypertrophic cardiomyopathy masked by pericarditis
DOI:
https://doi.org/10.4322/acr.2019.113Keywords:
Hypertrophic cardiomyopathy, Pericarditis, AutopsyAbstract
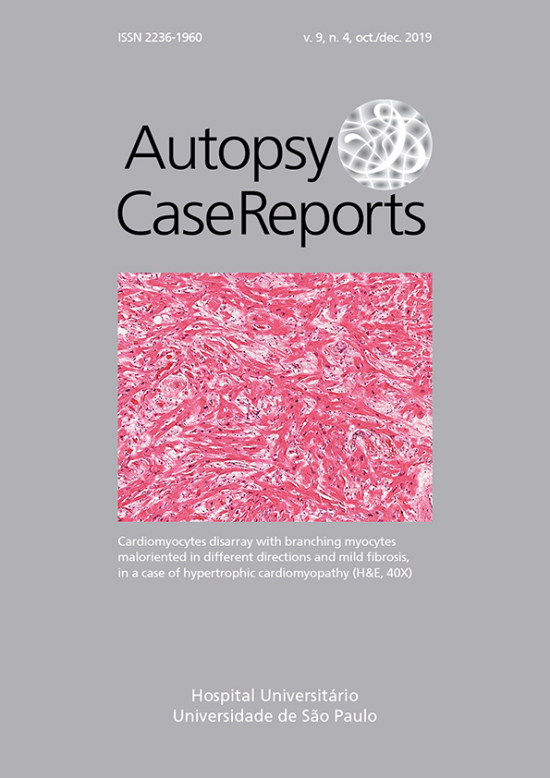
Hypertrophic cardiomyopathy used to be regarded as a rare untreatable cause of sudden death in young male athletes. This report is the case of a middle-aged female patient with hereditary hypertrophic cardiomyopathy masked by superimposed pericarditis and revealed by autopsy. This case report illustrates how co-morbidity can hide a crucial diagnosis. This case report also illustrates the value of autopsy disclosing a familial disease that is increasingly recognized and dramatically more treatable than a few decades ago. Sudden death due to hypertrophic cardiomyopathy has become preventable, if the diagnosis is made soon enough. The lessons for patient care from this case include the importance of not missing the diagnosis of hypertrophic cardiomyopathy in female patients.
Downloads
Published
Issue
Section
License
Copyright
Authors of articles published by Autopsy and Case Report retain the copyright of their work without restrictions, licensing it under the Creative Commons Attribution License - CC-BY, which allows articles to be re-used and re-distributed without restriction, as long as the original work is correctly cited.